Advance Care Planning - My Wishes, ReSPECT Plan, Anticipatory Medications
- Site:
- NHS Herefordshire & Worcestershire Integrated Care System Academy Exchange
- Course:
- PEoLC Resources
- Book:
- Advance Care Planning - My Wishes, ReSPECT Plan, Anticipatory Medications
- Printed by:
- Guest user
- Date:
- Tuesday, 14 October 2025, 7:13 PM
Advance care planning (ACP) is a voluntary process. It gives patients an opportunity to share their wishes and preferences for future care, based on what matters most to them. Documenting this helps guide future health care. This can be important if you become too poorly or are unable to make or express choices at the point of care.
People who have completed advance care planning tell us how it reassures them to know that their individual wishes are documented and how this can influence their personalised care.
Advance care planning also supports friends and family during times of crisis, by ensuring that those important to the patient can see preferences for care, relieving them of the burden of uncertainty.
This process may involve more than one conversation over time and can be with whoever the patient wants to involve.
Herefordshire and Worcestershire - Dying Well (icb.nhs.uk) has a short introduction to advance care planning where you can find some helpful videos.
Why Plan Ahead? - NHS
 |
 |  |
|---|
My Wishes
Advance statement about your wishes - NHS
Final 12 Advance Statement PDF
A small number of hard copies are available and have been distributed to local providers. If you require signposting to hard copies, please contact PEoLC team at ICB. M.carpenter@nhs.net
My Wishes Easy Read Information
Universal Principles For Advance Care Planning Easy Read
Coming soon:
Digital version on patient portal which will be completed by patient electronically and shared as pdf.
Patient Portal :: Herefordshire and Worcestershire Integrated Care System
 |
 |  |
|---|
ReSPECT Plan
ReSPECT stands for Recommended Summary Plan for Emergency Care and Treatment.
ReSPECT is a national initiative which documents individualised recommendations for a person’s clinical care in emergency situations when they do not have capacity to make or express choices.
Such emergencies may include death or cardiac arrest but are not limited to those events. The process is intended to respect both patient preferences and clinical judgement. The agreed realistic clinical recommendations that are recorded include a recommendation on whether or not CPR should be attempted if the person’s heart and breathing stop.
1.Joe’s ReSPECT journey - Joe's ReSPECT Journey videos, a ReSPECT explainer for healthcare professionals.
2. Examples of completed ReSPECT Forms v1-4. Four examples of how to complete the new ReSPECT form for patients.
- Respect v1 Respect-v1.pdf
- Respect v2 Respect-v2.pdf
- Respect v3 Respect-v3.pdf
- Respect v4 Respect-v4.pdf
•Joe’s ReSPECT Journey- a
ReSPECT
explainer for healthcare professionals
The
ReSPECT process creates personalised
recommendations for a person’s clinical care and treatment in a future
emergency in which they are unable to make or express choices.
Follow
Joe’s journey through the ReSPECT
process, and watch how he develops a plan
with healthcare professionals that respects his wishes and needs.
This video is aimed at healthcare professionals who may need to support patients who have or want a ReSPECT form.
•ReSPECT guide for clinicians - A Guide from the Resuscitation Council UK for clinicians completing the plan.
Guidance-for-Clinicians.pdf
ReSPECT useful phrasing when writing a plan
•Dying
for Beginners/ Dr Kathryn Mannix
A short animation by Emily Downe, and voiced by Dr Kathryn Mannix which guides you gently on a step by step journey through the process of dying
•Heart Stopping Moments
Dr
Kathryn Mannix draws upon her life's experience as a Palliative Care Physician
to explain 'ordinary dying' and why CPR is both important and when an
appropriate course of life saving action
 |
 |  |
|---|
Anticipatory prescribing of ‘just in case’ medicines is an important part of end-of-life care, which enables prompt symptom relief at whatever time the patient develops symptoms that cannot be managed by oral medications.
Advance care planning should include anticipatory medicine prescribing. This prevents delays in clinicians administrating by ensuring there is a supply of drugs and administration charts available for use in the patient’s home, for when they are needed.
An audit of PCN prescribing identified a variety of medicines, doses, strengths and frequency were being prescribed. This highlighted a need for recommendations and guidance for generalist prescribers, who may only prescribe anticipatory medicines infrequently.
Generalist and specialist palliative clinicians have collaborated to create an EMIS prescribing protocol and supporting documents, which are designed to improve symptom control for patients who are at End-of-Life, to enable more timely administration, more equitable access and to reduce prescribing and administration errors.
The anticipatory medicine protocol is for use by PCNs and OOH providers in Herefordshire and Worcestershire, or anyone who is prescribing anticipatory medicines for patients in their own home or a community residential setting.
The prescription and prescription chart are generated digitally through EMIS Web, or the protocol can be imported into a compatible system. The protocol at the point of use with the patient, is a paper process and copies of documents are left in the patient’s home.
Anticipatory Medicine Protocol
2 Elements
- EMIS
web or imported prescribing protocol – generates digital prescription
& prescription chart to be printed or emailed
- Supporting
guidance and administration documents - ALL to
be printed as a pack and left in patient’s home
- Prescriber
and Administrator Guidance for Subcutaneous Anticipatory Medications PRN &
Syringe Pump
- Administration
Record for Subcutaneous PRN Medicines
- Administration
Record for Syringe Pump Medicines
- Syringe
Pump Observation Chart
- Record
of Medicine Stock
- Prescriber and Administrator Guidance for Subcutaneous Anticipatory Medications PRN & Syringe Pump
- Administration Record for Subcutaneous PRN Medicines
- Administration Record for Syringe Pump Medicines
- Syringe Pump Observation Chart
- Record of Medicine Stock
The prescribed medicines may include a dose range. Administrators should begin on lowest dose unless instructed otherwise & never administer outside of their competence. Appropriate training needs to be completed.
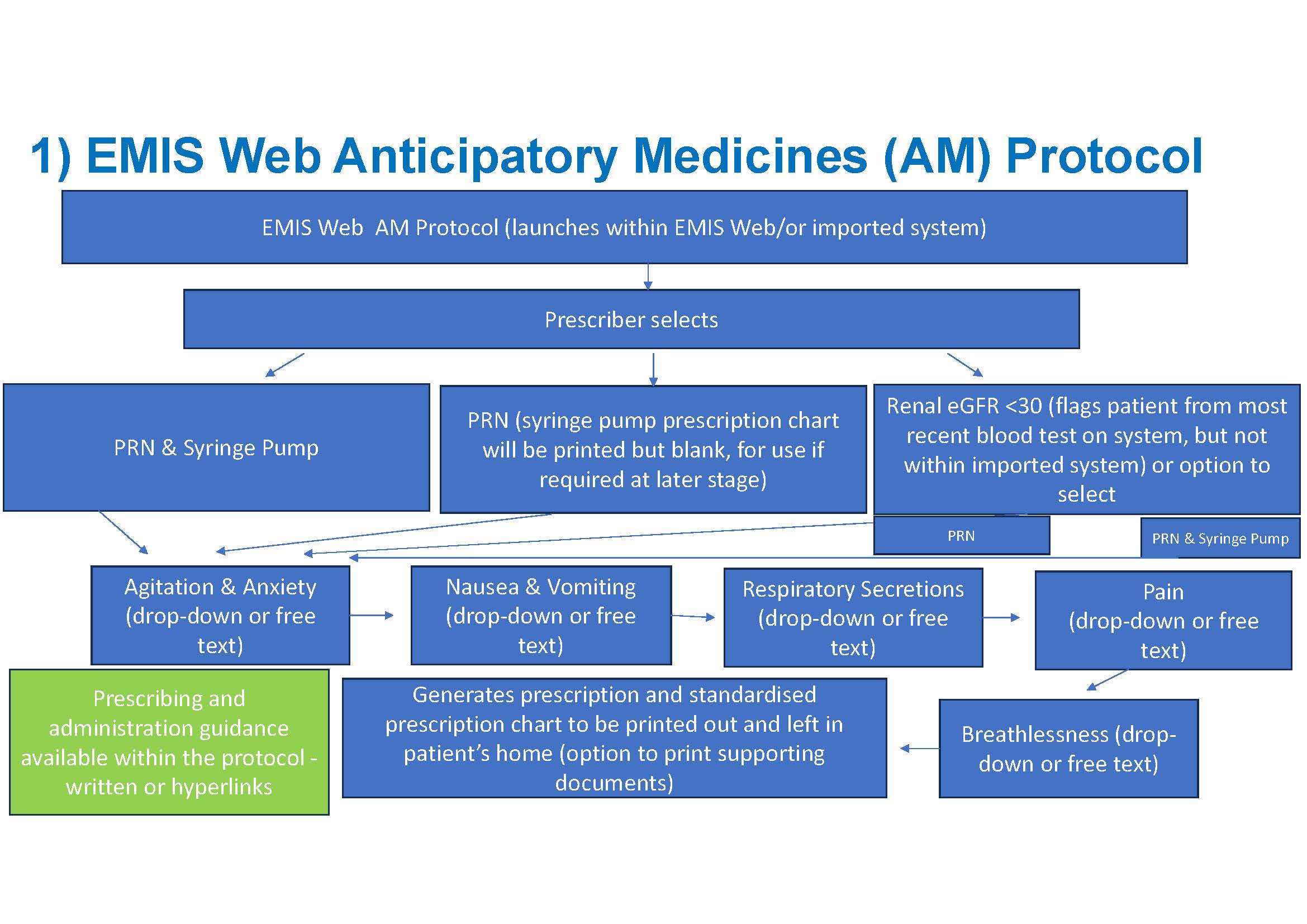
Protocol Paper Documents – Version 1.0 in use – ALL NEED TO BE PAPER COPIES IN PATIENT’S HOME